The virus that has been at the forefront of everyone's minds is the coronavirus, and while it has caused disruption to our daily lives, there are also other viruses that we should take note of before they impact our health.
In this segment, we will be looking at the role in which viruses play in the formation of cervical cancer.
Virus and cervical cancer
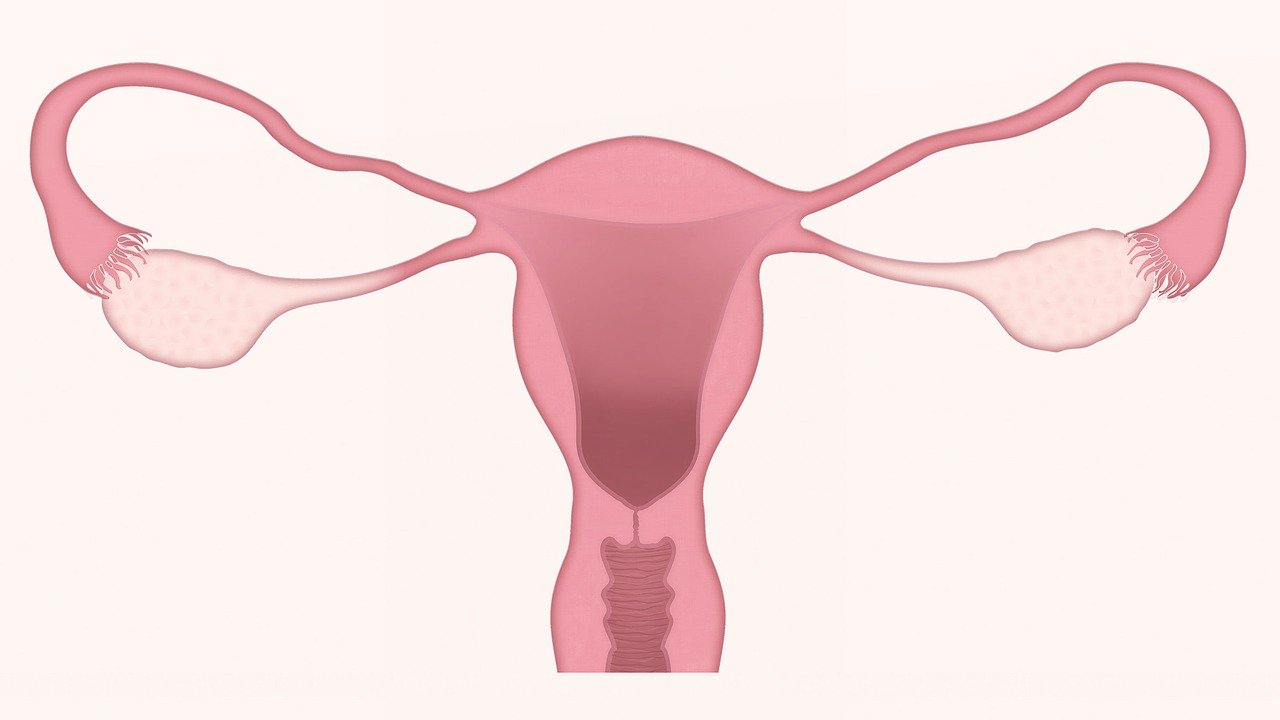
Dr Wong Chiung Ing, Senior Consultant and Medical Oncologist at Parkway Cancer Centre, shared with us what the human papillomavirus (HPV) is, and how it's linked to cervical cancer.
HPV is the most common sexually-transmitted infection, and "up to 80 per cent of women who are sexually active will become infected," said Dr Wong.
She added: "HPV infection accounts for 99 per cent of all cervical cancer, the organ connecting the uterus and the vagina. Two HPV types (16 and 18) cause 70 per cent of all cervical cancers."
In 2018, an estimated 570,000 women were diagnosed with cervical cancer worldwide, and about 311,000 women died from the disease, as reported by the World Health Organisation (WHO). As such, it has been identified as the fourth most common cancer in women.
In a large majority of cases, about 80 to 90 per cent of the infections are transient, and the body's immunity system is able to fight and clear off the virus.
But in a minority of cases, when the HPV virus stays in the cervix and causes persistent infection, it can result in abnormal growth in the cells of the cervix's inner lining.
"These cells can then develop into pre-cancerous cells called Cervical Intraepithelial Neoplasia (CIN), which can eventually develop into malignant cancer," explained Dr Wong.
The process may take up to 20 years before it becomes cancerous, and in most cases, the infection starts when the women are in their 20s, leading up to the pre-cancerous stage in their 30s, and develops into cancer in their 40s.
While 90 per cent of the HPV infection will clear up on its own and not all cases will become cancerous, some will lead to skin growths on the genitals or become genital warts, which can be painful or uncomfortable.

On the question about who has a higher risk of contracting cervical cancer, Dr Wong said: "Women who are sexually active face a higher risk of HPV and, therefore, cervical cancer."
Women who contracted sexually transmitted diseases such as herpes, chlamydia and gonorrhoea are also at a higher risk of having cervical cancer. Those with multiple sexual partners, or whose partners have many other partners, and women who've had unprotected sexual intercourse at an early age, are also at risk.
Said Dr Wong: "Women with a weak immune system such as HIV patients, transplant patients and patients with autoimmune diseases also face greater risk."
Symptoms and treatment
There are no obvious signs and symptoms when you have an HPV infection. Symptoms may not also be obvious during the pre-cancerous changes, and in some cases, in the early stage of cervical cancers too.
"In many cases, symptoms may develop only when the cancer cells start to invade the surrounding tissues." Said Dr Wong.

Some signs and symptoms to look out for include abnormal vaginal bleeding including bleeding after intercourse, bleeding between periods or after menopause. Other symptoms include bloody, heavy or smelly vaginal discharge.
Painful or difficult urination, leaking of urine or faeces from the vagina, pelvic/back pain and chronic constipation and feeling of the presence of stool despite having emptied your bowels could also be signs of advanced cervical cancer.
Women suspected of having cervical cancer should undergo biopsy for confirmation of diagnosis; they then have to go through careful clinical examination, followed by scopes to obtain biopsy samples of the tumour.
"When the diagnosis is confirmed, scans such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT) and Positron Emission Tomography (PET) are useful to confirm the stage of the tumour," said Dr Wong.
Treatment options for CIN include ablative methods such as cryotherapy, laser vaporisation or coagulation. The other treatment option is excision using LEEP (Loop Electrosurgical Excision Procedure), laser or knife cone biopsy. These treatments can often be done as a day surgery procedure.
For the treatment of cervical cancer that invades deeper into the cervix, surgery, radiotherapy, chemotherapy, targeted therapy and immunotherapy are administered. These treatment options are dependent on the patient's stage of the disease.
"When diagnosed, cervical cancer is one of the most treatable forms of cancer, as long as it is detected early and managed effectively," according to WHO.
Prevention and cure

Women who have had sexual activity should begin cervical cancer screenings at age 25.
Dr Wong listed the frequency in which women should be getting a Pap test or HPV test.
● If you are between age 25 and 29, you should get a Pap test every three years
● If you are above 30 years old, you should get an HPV test every five years
While HPV infection cannot be treated, one can reduce the risk of infection and developing HPV-related cancers by going for vaccinations.
The HPV vaccines are effective against the strains of HPV viruses responsible for 70 to 85 per cent of all cervical cancers. These vaccines can be given early to girls from as young as 9 years old to women aged 26, and they work best before the start of any sexual activity.
Even though you've been vaccinated, Dr Wong advised that regular cervical screening tests is still necessary as it will help detect early changing cells that may turn into cancer.
"It is important to remember that vaccination does not guarantee that a woman will not get HPV infection or be spared of cervical cancer. This is because there are other HPV strains that may cause cervical cancer which will not be covered by the HPV vaccine," she added.
To reduce exposure to HPV infection and the risk of cervical cancer, Dr Wong also advised altering sexual behaviour and using condoms to prevent any sexually transmitted diseases, including HPV. It is also important to have primary prevention of cervical cancer by going for vaccinations, and secondary prevention by going for regular cervical screenings.
This article was brought to you in partnership with Parkway Cancer Centre.
